Santiago Nariño raised this question in a lecture. When we design healthcare systems within our organizations, do we think about all vulnerable populations? We often remember the poorest people, those who are not white. Still, there are many other vulnerable populations that we sometimes forget to consider in our services when designing our processes.
What, then, is equity in health?
“Equity in health: everyone should have a fair chance to achieve their full health potential, and no one should be held back from achieving this potential.” – Professor Margaret Whitehead, head of the WHO Collaborating Centre for Social Determinants of Health
Equity in the organization:
- More people with more opportunities
- More people with personal mobilization
- Greater diversity of ideas and recognition of the structural
- More space for care
Clinical equity:
- Better data for learning
- Intentional processes with equity
- Less variation in outcomes
- Better outcomes for all
Health equity (population):
- Better health, prevention
- Better health for longer
- Greater possibility of well-being
- Better social climate and social capital for all
The Institute for Healthcare Improvement (IHI) has already added EQUITY as the 5th goal to be achieved to improve healthcare.
Now it is up to each of us, stakeholders in the healthcare system, to pursue this in our work environment.
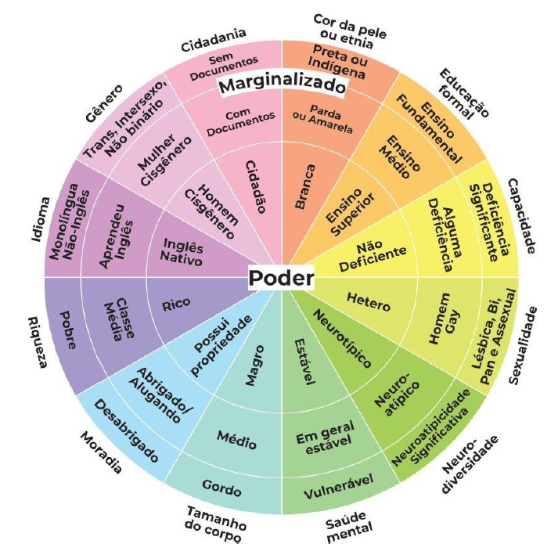
Legend
Power
Poor
Middle class
Rich
Homeless
Sheltered/Renting
Owns property
Fat
Medium
Thin
Vulnerable
Generally stable
Stable
Neurodiversity
Significant neuroatypicality
Neuroatypical
Neurotypical
Sexuality
Lesbian, bi, pan, and asexual
Gay man
Heterosexual
Ability
Significant disability
Some disability
Not disabled
Formal education
Elementary school
High school
Higher education
Marginalized
Skin color or ethnicity
Black or Indigenous
Mixed race or Yellow
White
Citizenship
Without documents
With documents
Citizen
Gender
Trans, Intersex, Non-binary
Cisgender woman
Cisgender man
Language
Monolingual non-English
Learned English
Native English